Diabetic Retinopathy
If you have diabetes mellitus, your body does not use and store sugar properly. Over time, diabetes can damage blood vessels in the retina, the nerve layer at the back of the eye that senses light and helps to send images to the brain. The damage to retinal vessels is referred to as diabetic retinopathy.
Nonproliferative Diabetic Retinopathy (NPDR)
NPDR, commonly known as background retinopathy, is an early stage of diabetic retinopathy. In this stage, tiny blood vessels within the retina leak blood or fluid. The leaking fluid causes the retina to swell or to form deposits called exudates.
Many people with diabetes have mild NPDR, which usually does not affect their vision. When vision is affected, it is the result of macular edema and/or macular ischemia.
Macular edema is swelling, or thickening, of the macula, a small area in the center of the retina that allows us to see fine details clearly. The swelling is caused by fluid leaking from retinal blood vessels. It is the most common cause of visual loss in diabetes. Vision loss may be mild to severe, but even in the worst cases, peripheral (side) vision continues to function. Laser treatment can be used to help control vision loss from macular edema.
Macular ischemia occurs when small blood vessels (capillaries) close. Vision blurs because the macula no longer receives sufficient blood supply to work properly. Unfortunately, there are no effective treatments for macular ischemia.
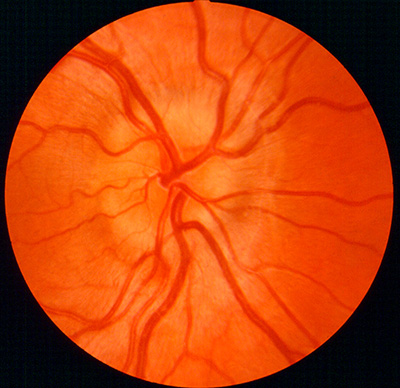
Fluorescein Angiogram — a test that will identify PDR symptoms.
Proliferative Diabetic Retinopathy (PDR)
In PDR, the retinal blood vessels are so damaged they close off. In response, the retina grows new, fragile blood vessels. Unfortunately, these new blood vessels are abnormal and grow on the surface of the retina, so they do not supply the retina with blood.
Occasionally, these new blood vessels leak and cause a vitreous hemorrhage. Blood in the vitreous, the clear gel-like substance that fills the inside of the eye, blocks light rays from reaching the retina. A small amount of blood will cause dark floaters, while a large hemorrhage might block all vision, leaving only light and dark perception.
The new blood vessels can also cause scar tissue to grow. The scar tissue shrinks, wrinkling and pulling on the retina and distorting vision. If the pulling is severe, the macula may detach from its normal position and cause vision loss.
Laser surgery or injection of medication into the eye may be used to shrink the abnormal blood vessels and reduce the risk of bleeding. The body will usually absorb blood from a vitreous hemorrhage, but that can take days, months or even years. If the vitreous hemorrhage does not clear within a reasonable time, or if a retinal detachment is detected, an operation called a vitrectomy can be performed.
People with PDR sometimes have no symptoms until it is too late for treatment. The retina may be badly injured before there is any change in vision. There is considerable evidence to suggest that rigorous control of blood sugar decreases the chance of developing serious proliferative diabetic retinopathy.
Because PDR often has no symptoms, if you have any form of diabetes you should have your eyes examined regularly by your eye doctor. An eye examination is the only way to find changes inside your eye. If your eye doctor finds diabetic retinopathy, he or she may order color photographs of the retina or a special test called fluorescein angiography to find out if you need treatment. In this test a dye is injected in your arm and photos of your eye are taken to detect where fluid is leaking.
If you have diabetes, early detection of diabetic retinopathy is the best protection against loss of vision. You can significantly lower your risk of vision loss by maintaining strict control of your blood sugar and having your eyes checked regularly. People with diabetes should schedule examinations at least once a year. Pregnant women with diabetes should schedule an appointment in the first trimester because retinopathy can progress quickly during pregnancy. More frequent medical eye examinations may be necessary after the diagnosis of diabetic retinopathy, with the goal of diagnosing progression of the disease before the vision is affected.
A recent innovation to help individuals better manage their blood sugars is the use of continuous glucose monitors, such as the Abbott FreeStyle Libre. These are sensors that attach painlessly to the upper arm to monitor the blood sugars. The data can be read on a specialized reader or on a smartphone using a free app. These give detailed information about blood sugar levels throughout the course of the day without requiring frequent finger sticks. By informing patients and their doctors, they help with blood sugar control. In Ontario, they are covered for patients diagnosed with diabetes mellitus.
